At an early August lunch, Tabitha McIntosh suddenly saw nothing but white. She experienced vertigo and felt sick and thought she had a migraine — what she believed was thanks to hormonal changes due to perimenopause.
“I’ve never had a migraine before, but I know plenty of people who have,” McIntosh, 50, of London, told TODAY via email. “They are associated with hormone shifts and perimenopause, so I assumed this was a migraine aura.”

After days with a headache and worsening symptoms, she went to the emergency room and doctors sent her home, ruling out a stroke. The next day, she struggled to get dressed and could no longer type normally. Two days after her first hospital visit, she returned with proof that something was wrong. She underwent a CT scan and she learned the reason for her non-stop headache.
“(An) A&E doctor, who seemed surprised when he brought the scan up on the screen … said, ‘You’ve had a stroke in your parietal lobe,’” she said. “The paramedic who arrived in the ambulance to transfer me said, ‘I’ve never had a walking, talking patient before today.’”
Headache and hormones
On August 4, McIntosh’s experienced a “white out” headache. While ibuprofen and rest helped, the pain never subsided. Still, she joined friends for dinner that evening.
“I woke up two hours later with restored vision but an insistent throbbing headache on the right side,” she said. “My headache never went away, but it wasn’t intrusive enough to interfere with the evening. I spoke to both women since and they both agree that absolutely nothing about my behavior, manner, mood or ability to handle cutlery was in any way notable or different.”
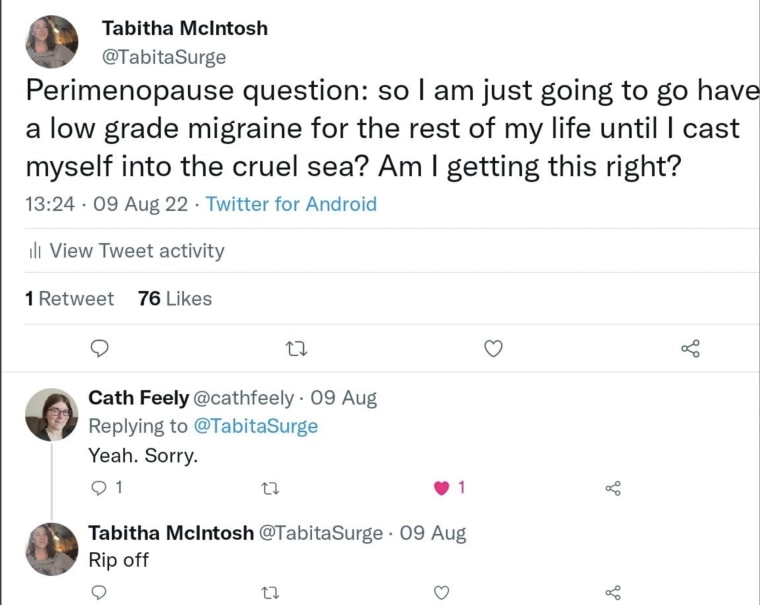
She didn’t think a consistent “low-level headache” was reason to call her doctor but by August 9, she felt frustrated by the constant pain. So she asked Twitter if her persistent headache a symptom of perimenopause.
“As you can see from the dozens of women who replied to my tweet, hormone-driven headaches are a very common fact of perimenopausal life,” McIntosh said. “I assumed it was perimenopause and because I framed it that way so did everyone who replied.”
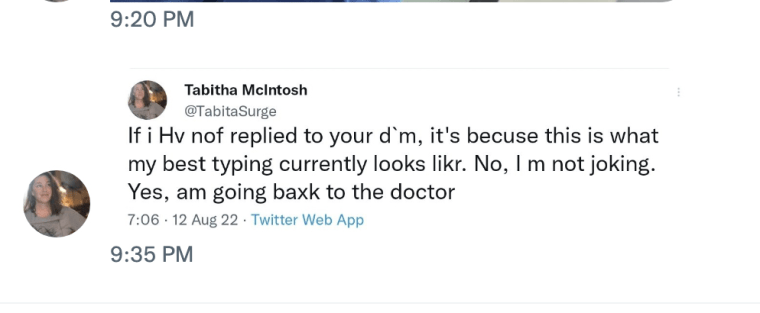
The next day, though, McIntosh noticed new and upsetting symptoms, which she also shared on Twitter:
“Day 9 of migraine: can no longer type without slow effort or coordinate left and right sides. Tragic impact on my ability to function, care for my mother, dress, self tweet spicy takes. Perimenopause is hell.”She struggled typing and texting became “almost impossible.” It took her two minutes to type her tweet. She fumbled to put on a crossbody purse because she couldn’t figure out where to put her arm and it hung limply around her neck. Getting into a bra took her three minutes and she put her jeans on backwards.
“It’s hard to describe," she said. "I could do things—there was nothing wrong with my strength — but I couldn’t work out how to do them."
She visited her doctor on day 11 of her headache, which was “throbbing behind my right temple that extended back across the top of my head.” She walked one mile to the appointment, where she hoped her doctor would adjust her hormone replacement therapy to ease her pain. Getting to the office felt difficult.
“My left arm swung into a sign outside a store and a trash can,” she explained. “I wasn’t able to judge distance or complete what should have been automatic motions with that hand.”
Her doctor asked McIntosh to smile, frown, follow a moving object with her eyes and put her arms out, among other tasks, to assess her for stroke. McIntosh easily completed all the tests.
“Then she asked me to copy her in laying my left hand palm-side up on my right hand and flipping it over so my hands were palm-to-palm,” she said. “I had no idea what to do.”
Her doctor felt alarmed by McIntosh’s lack of coordination and sent her to the accident and emergency (A&E) department. The A&E doctor performed the same stroke tests there.
“(He) couldn’t see any neurological abnormalities. He recommended paracetamol and codeine instead of ibuprofen and told me not to hesitate to come back if my symptoms worsened or if I experienced dizziness,” McIntosh recalled. “He then said that they could send me for a scan if I was really concerned but that he couldn’t see any need for it. In a decision I regretted almost immediately, I deferred to his judgment and went home.”
The next morning, McIntosh faced more difficulties.
“When I tried to pull my trousers up, I found myself tugging on my T-shirt instead. It was surreal and disorienting — like being through a looking glass and not being able to understand what was reflection and what was reality,” she said.
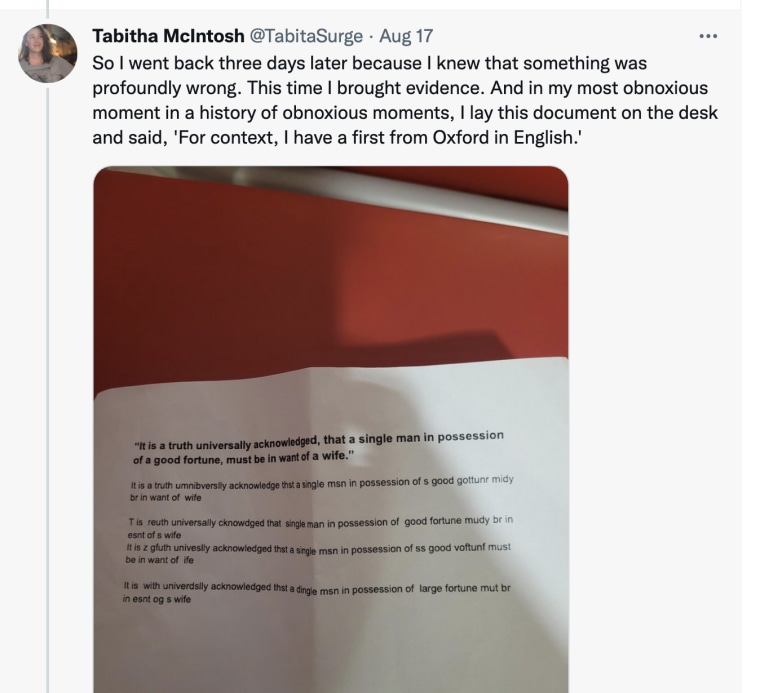
She returned to the A&E department with proof, a poorly typed sentence that should have been easy for her to accomplish. She had gone through the stroke assessment twice and passed so she though the doctors needed more information.
“My typing was the most obvious symptom,” she said. “I choose my typing as evidence.”

The nurse told her to show the doctor because she believed McIntosh needed a CT scan. While the doctor asked her to go through the stroke assessment again and suggested that stress could be to blame, he ordered a CT scan. That’s when McIntosh learned she had had a stroke.
“I had no idea that the very odd and vague symptoms I was experiencing were symptoms of a stroke,” she said. “I have spent all my life being trained to ignore pain and brain fog and discomfort, to put it all down to hormones and difficult female bodies and when I was most in physical emergency, I did it to myself. In effect, I medically gaslit myself.”
Raising awareness
McIntosh shared her experience on Twitter, in part, to educate others about atypical stroke symptoms and to encourage others not to downplay any worrisome changes to their health.
“Being in your 50s and female is not an explanation for everything happening to you,” she said. “You have to be your own best advocate. You may also have to be your own best detective.”
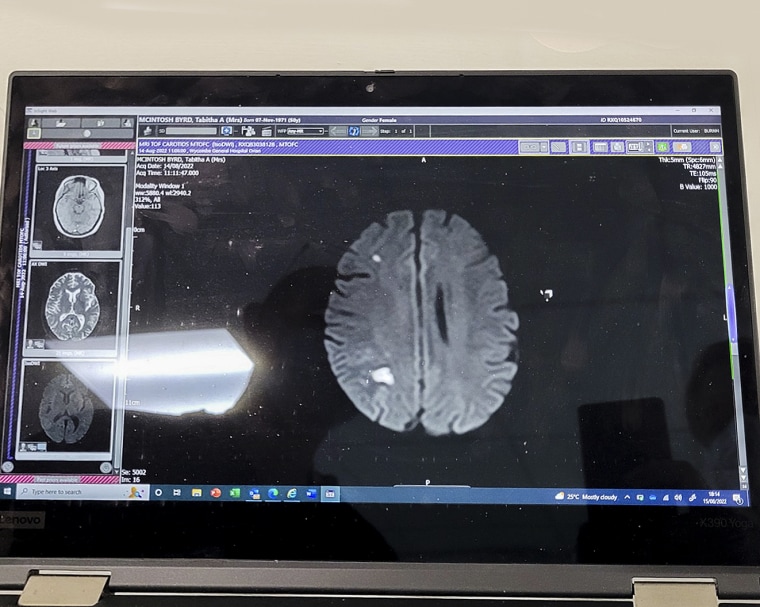
McIntosh’s “oddest symptoms” have improved. She’ll be taking blood thinners to prevent clots for the remainder of her life and needs to undergo more scans and examinations so doctors can determine why she experienced stroke.
“I have spent all my life being trained to ignore pain and brain fog and discomfort, to put it all down to hormones and difficult female bodies and when I was most in physical emergency, I did it to myself. In effect, I medically gaslit myself.”
“The brain is a remarkable organ, and is extremely effective at working around damage and finding new pathways,” she said. “The chief problem now is dread. Fear of having another stroke is always present — for the first few days I was convinced I would die in my sleep.”
In some ways, she’s not surprised her thread about stroke was so popular.
“It’s like a Gothic horror — the idea that you can have a massive brain injury and not know it all; that you can keep walking and talking while part of your brain is screaming and dying from lack of oxygen.”