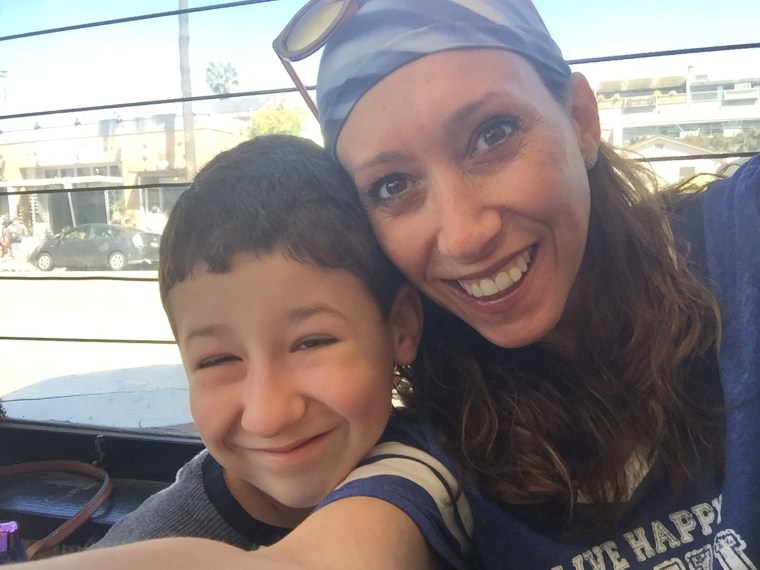
After Heather Osterman’s son, Max, now 13, was born, she learned he had a genetic condition called Prader-Willi syndrome. While she and her husband were able to connect Max to all the therapies and treatments he needs, there’s one aspect of the condition that remains uncontrolled — Max’s insatiable hunger. There's no treatment for it; people with Prader-Willi syndrome feel starved constantly and can’t be left unattended with food.
“It’s not just that you’re hungry,” Osterman, 52, from the Chicago area, tells TODAY.com. “(The hunger is) like, ‘I’ve been walking through the desert for seven days, and my body is shutting down I’m so hungry. I’m so ravenous I could eat out of the garbage.’”
Osterman is sharing Max’s story to raise awareness of the rare condition.
“It’s important for people to know that there’s so many things out there that people struggle with,” she says. “Look to see people for more than face value.”
An ongoing struggle with food
It was clear Max had health struggles almost as soon as he was born. After Osterman delivered him via C-section, she finally got to hold him, and he was “very limp," she recalls.
“I got to say, ‘Hi,’ to him for a minute and then they took him to the NICU,” she says. “I never really got to have that moment with him.”
For two months, Max stayed in the neonatal intensive care unit, where he “checked the box for Prader-Willi,” but, for reasons Osterman doesn’t know, he wasn’t yet diagnosed with the condition.
“He had low muscle tone, failure to thrive. He couldn’t eat on his own," Osterman says. He had a tube in his stomach to help him eat for about a year. “We did intensive training, like every day, to help him learn how to feed himself without choking because he silently aspirated," she adds.

A scan also showed he had some brain damage. Doctors treated him for each of the symptoms. When he was 18 months old, Max’s neurologist tested him for various conditions, and that’s when Osterman learned Max had Prader-Willi syndrome.
“I did what every doctor will tell you not to do, which is go online and Google Prader-Willi syndrome,” she says. “The list has every horrifying thing that you could possibly imagine that your child will have or won’t be able to do.”
Luckily, many of the therapies Max received were ones he needed to thrive.
“We were doing everything we were supposed to do,” Osterman says. “The only thing we were really missing, which was a pretty big piece in my opinion, is that growth hormone.”
Children with Prader-Willi are often shorter in stature, so treatment includes growth hormone to help them physically developed, according to the National Library of Medicine.
“He was a little over 2 years old by the time we actually got him on growth hormone,” Osterman says. “We missed about two years of treatment.”
It has helped Max grow and develop, and “it helps with (his) overall functioning.” Those with Prader-Willi syndrome often have mild cognitive impairment, as well, and Max faces challenges with motor skills. Still, he often surprises his family and doctors.
“Max has just proven himself. He always exceeds the expectations that anybody’s ever had,” Osterman says. “It’s been really, truly amazing to watch. But the one thing we can never get around — or at least we’ve not been able to get around so far — is the hunger.”
Children with Prader-Willi syndrome “don’t have the ability to know that they’re full,” Osterman says. They have slower metabolisms, and their stomachs do not empty normally, so they frequently have food in their stomach. Their hypothalamus, the area which controls hunger in their brains, doesn’t work like it does in other people. Their brains always tell them they’re hungry.
“Max pretty much thinks about food from the minute he wakes up until the minute he goes to bed,” Osterman says. “It’s challenging because the amount of anxiety that surrounds him and, of course, the family (is high). We’re worried about what he’s going to eat and when he’s going to eat … He’s worried about it.”
This means Max needs constant supervision to avoid overeating.
“You can technically eat ... until your stomach ruptures,” Osterman says.
If the family wants to go to a restaurant for dinner, Max begins obsessing over it. He’ll think about what he will eat and how big portions will be. Osterman also has to plan for what happens if the portion is bigger than they thought it was and how to not allow Max to eat everything.
“It’s a disaster. There’s a lot of planning that has to go on when you go out,” Osterman says. “If there’s a buffet, it’s a nightmare.”
Prader-Willi syndrome
Prader-Willi syndrome occurs when a baby is born missing their father’s 15th chromosome, says Dr. Jennifer Miller.
“It’s a random event in most cases” Miller, a pediatric endocrinologist at University of Florida, who also treats Max, tells TODAY.com. “It’s considered a rare disease. It’s one in 15,000 to 20,000.”
It’s most often diagnosed within the first few weeks of life, when doctors detect low muscle tone, little crying, problems eating and failure to thrive.
“The classic features in babies, interestingly, is that they do not want to eat, so they will push the bottle out of their mouth,” Miller says. “They have no desire to eat. They don’t cry for food.”
Most often the babies receive a G-tube to prevent them from dying. Doctors treat children with growth hormone to help them become taller and develop more muscle mass. It also bolsters cognition, helping many with the mild cognitive impairment.
The lack of interest in food from infants feels confounding because at age 4 or 5, they develop an increased interest in and awareness of food, Miller says, adding that by the time they’re 9, they develop hyperphagia, which is “uncontrollable appetite.”
“They eat anything and everything,” Miller says. “It’s an abnormal obsession.”
Hyperphagia makes people with Prader-Willi syndrome feel “anxious” and display “obsessive compulsive traits” about food, she says. Miller has had patients who have eaten food off the ground, consumed food out of garbage cans, ingested raw frozen chicken, stolen food, eaten 10 pounds of dehydrated potato flakes and even assaulted people who came between them and food.
“There’s no off-switch, so their brain doesn’t even say, 'You’ve eaten enough. Stop,’” Miller explains. “They can eat an ungodly amount of food," — anywhere from 10,000 to 20,000 calories if left unattended.
What’s more, these patients cannot vomit, she says, so there’s no biological mechanism standing between them and dangerously overeating.
“One of the biggest causes of death in people with (Prader-Willi syndrome) is actually the bursting of the stomach because they eat so much,” she says. “(Overeating) will actually rupture the wall of the stomach, and they become septic and die.”
While drugs like Ozempic work by targeting receptors in the brain to tell people they're not hungry, these class of medications will not work on people with Prader-Willi syndrome.
“It doesn’t really seem that those medicines will be efficacious because they don’t have those receptors for the medicine to hit in the brain to say, ‘Hey don’t think about food,’” Miller says.
Most families lock their food up to stop their child from overeating. Having structure also helps. While growth hormone helps people with Prader-Willi syndrome be able to attend higher education get a job, they cannot live unsupervised. Miller has had patients who go to college, for example, and spend all their time going from dining hall to dining hall to eat.
“It’s very lonely,” Miller says. “When you’re so focused on food, it is very, very difficult to be social to make friends. Nobody understands because nobody else cares about food as much as you do.”
Miller has been involved as a principal investigator in a clinical trial looking at a drug intended to stop the insatiable hunger. The research is ongoing.

‘Live life full’
The Ostermans often think of the mantra “live life full.”
“Live to your fullest potential (and) live life with a ... feeling that ... that you cannot be limited by your desire for something that’s harmful to you. Allow yourself to think of something else other than hunger.”
Max recently had his Bar Mitzvah and celebrated by visiting the TODAY show and meeting Hoda Kotb. He’s been a fan since she co-hosted the Fourth Hour of TODAY with Kathie Lee Gifford.
“We went there with the hopes of just saying hello to her and to get his picture with her,” she says. “She really decided to make his day magic.”
Osterman hopes Max's story encourages others to look past his condition.
“We wanted to show how amazing he is and how amazing he can be if we can help him to be able to live to his fullest potential,” she says. “We’re still fighting for that which will come in the form of finding something (to treat) his hunger.”
