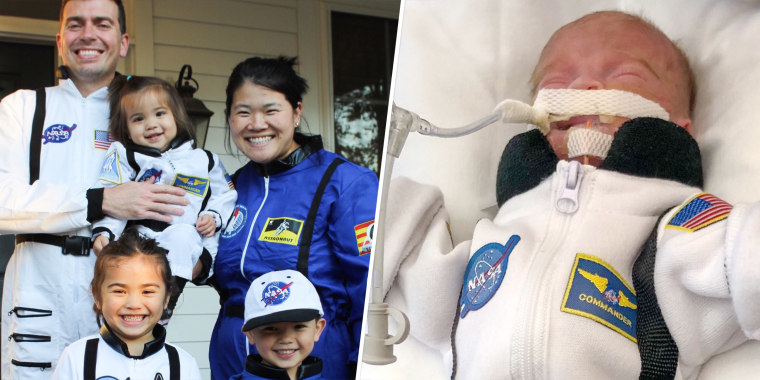
A year ago, Katy Crince gave birth to her fourth child, Bodyn, a micro-preemie weighing 1 pound 7 ounces. He immediately went to the neonatal intensive care unit (NICU) where he stayed for 139 days.
As the family prepares to celebrate Bodyn’s first birthday on Sept. 30, Crince reflects on what’s she’s learned as a NICU mom.
“For parents, it’s a very traumatic experience. They go through some PTSD or they feel a ton of grief or they feel a ton of anger. And to be honest with you, I never felt any of that,” Crince, 37, of Northern Virginia, told TODAY Parents. “I’m grateful for so many things — the NICU doctors and nurses, the respiratory therapists, the whole staff there. (I’m) grateful for all our friends and family and grateful that our son made it through.”

Early labor and a micro-preemie
When Crince was 10 weeks pregnant, she was at the playground when she noticed she was bleeding. She visited the emergency room because she worried she was miscarrying. An ultrasound showed that the baby was OK, but she learned she experienced something called a subchorionic hemorrhage. This occurs when blood pools between the membranes surrounding the fetus, according to National Library of Medicine.
“When they checked me again at 13 weeks everything had resolved itself and the hemorrhage had gone away,” Crince said. “I was told this isn’t really considered high risk. There’s no reason for this happening meaning anything for the future pregnancy. I still felt some anxiety.”
On Sept. 29, 2021, Crince went into labor.
“I have a placental abruption, which started to trigger my labor,” Crince said. “Looking back my OB thinks maybe the placenta was just not that great from the start, considering I had the hemorrhage and the placental abruption.”

She was only 23 weeks and 1 day pregnant when she gave birth. Doctors told Crince and her husband, Jonathan, that when a baby is that early parents decide what interventions the baby receives.
“I could still feel the baby kicking inside of me, his heart rate never dropped or anything. So I just took that as a sign that he was a fighter and we had to give him the best chance,” she said. “(We said), ‘Please do everything that you can to save him.’”
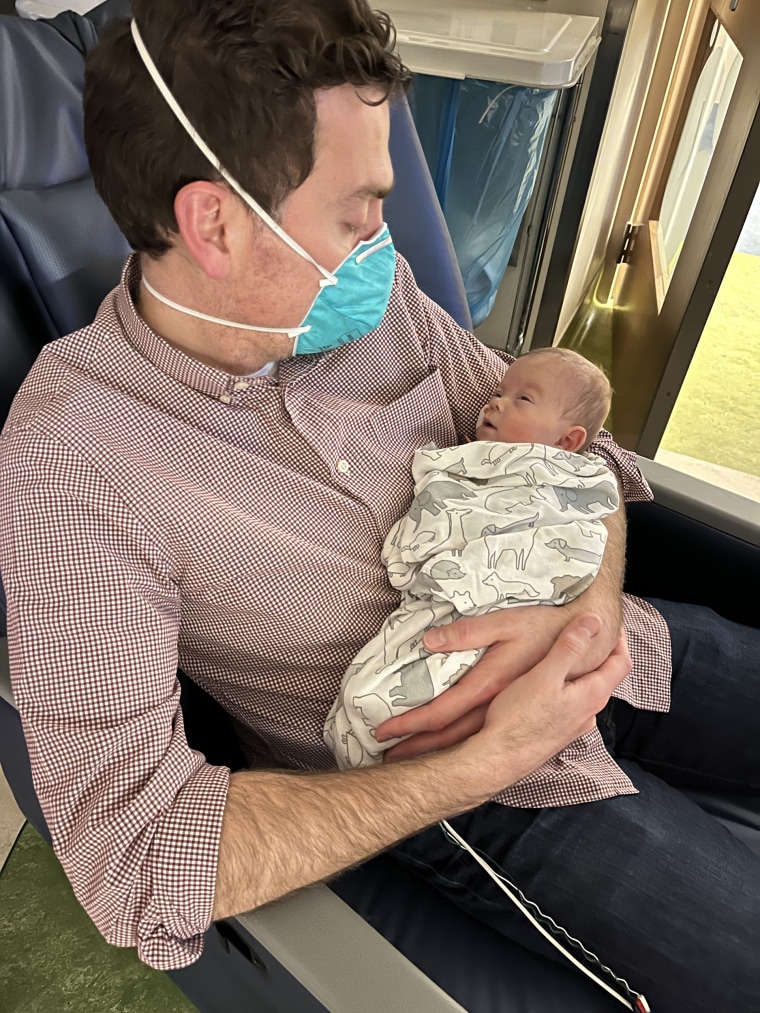
After Bodyn was delivered via C-section, the neonatologists intubated him. Crince couldn’t see him for 24-hours while she recovered.
“Nothing prepares you for seeing your baby so so so small,” she said. “They told us the best thing you can do for your baby is talk to him and he can feel your presence.”
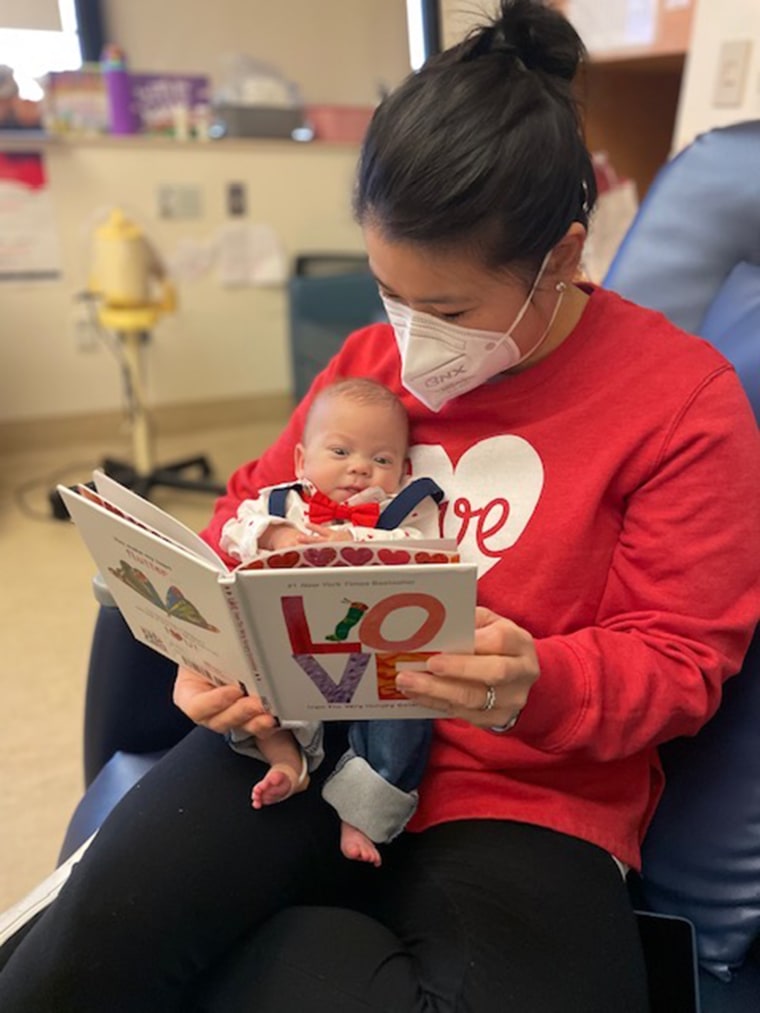
They would read to him and talk to him, anything they thought could give him “a fighting chance.”
“There were statistics saying the more present the parents were in the NICU rooms, the better the odds were for the baby outcomes,” she said. “He was in the NICU for 139 days and we missed — between my husband and I — only four or five total because of a COVID exposure.”

Doctors couldn’t insert a peripherally inserted central catheter, also called a PICC line, in Bodyn so they transferred him to Children’s National Hospital in Washington, D.C. A PICC line makes it easier for doctors to give babies medication and nutrition in a large vein in the chest, according to the Mayo Clinic.
Moving a baby that tiny could have been devastating.
“We prepared ourselves for that. We went in and we took pictures and pictures with him. They did footprints of his feet,” Crince said. “The nurse was amazing and walked us through it.”
Bodyn survived but soon after a nurse noticed “dark coloration” on his skin near his groin that indicated he might have air trapped in his belly. Doctors created holes for the air to escape but then his blood levels lowered and his blood pressure became erratic.
“They needed to go in and do an emergency surgery to see what was going on,” Crince said. “The neonatologist came out and told us he found some perforations in his bowels, which was called NEC.”
Necrotizing enterocolitis (NEC) occurs in premature babies where parts of their intestinal tissue can die, according to the Cleveland Clinic. Doctors tried to reduce this with surgery.
“His bowels are outside of his body for a few days to see if that would allow these perforations and bowels to heal,” she explained. “When they had gone in they had found some dark spots on his bowels and basically with NEC it eats away at your bowels and a lot of times they have a very very short amount of time to get in and operate.”
But, removing parts of the bowels can cause other health complications, such as short bowel syndrome or the need for a lifelong feeding tube, Crince said.
“It was those tough conversations that we had to have like how far are we going to let them go to save our child’s life, but also knowing we didn’t want him to suffer too much,” she said.
Luckily doctors did not have to remove any of his bowel and created an ileostomy, an opening in the abdomen that helps waste move through the body if the colon isn’t working correctly.
“That initial nurse saved him in a way of noticing right away,” she said. “Miraculously, through all of this he didn’t have to have any of his bowel removed.”
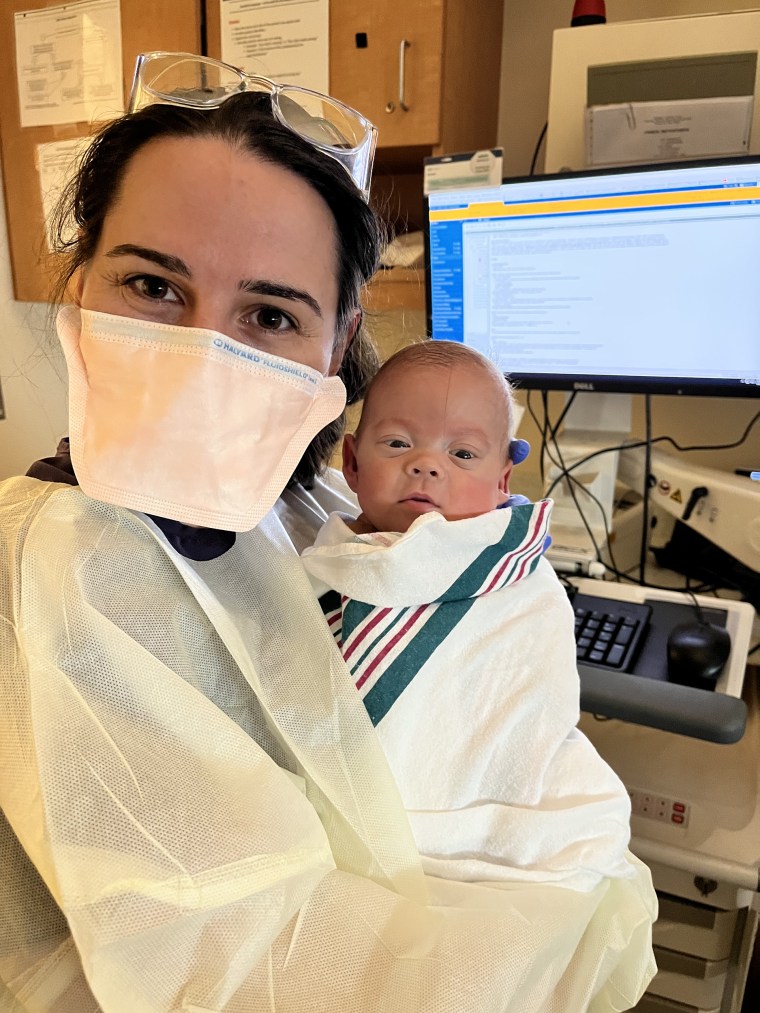
When Bodyn was about 100 days in his NICU stay, doctors reconnected his bowel and closed his ileostomy. He also experienced two brain bleeds and developed hydrocephalus. Doctors thought he might need to undergo brain surgery to ease the built-up pressure, but antibiotics treated an infection and reduced the swelling.
“Even though he was so small, the lungs were never really our big issue and the heart wasn’t ever an issue,” Crince said.
The family credits the nurses with Bodyn’s success. One nurse, Robyn, often did special things with him for mom and dad.
“She had made little footprint signs with him,” Crince said. “I appreciated whenever she was his nurse because the next day I would come in and see all the things she would do for him.”
'Typical fourth kid'
After 139 days in the NICU, Bodyn came home the day after Valentine’s Day. He still has occupational and physical therapy. They’re trying to encourage him to eat solid foods but so far he’s “not too interested.” He sees a neurologist because he’s at risk for cerebral palsy, but otherwise fits right in with his siblings.
“(He’s) your typical fourth kid, like super chill. He only gets upset if he’s hungry or tired,” she said. “He’s very smiley.”
For premature babies doctors consider an adjusted age. So even though Bodyn will be 1 on Sept. 30, he’s considered 8 months old.
“He’s probably developmentally even a little bit delayed from there,” Crince said. “From not being able to hear him cry for months in the NICU to now being able to hear him laugh is just so incredible to us.”