From infected restaurant workers to tainted frozen berries, the threat from hepatitis A continues to cause alarm in communities across the country.
The latest scare involves a food handler at a ShopRite in Somerville, New Jersey, who worked at the store while contagious during the second half of October, the state's department of health announced this week.
The agency urged customers to throw away any deli food they bought at the location during that period and get vaccinated as soon as possible if they did eat any of the items or used the store's restrooms during that time.
“I’d be surprised if there’s anybody in Somerville who hasn’t been to this store recently,” Jim Meirose, a Somerville resident, told NJ.com. Hundreds of people have been waiting in line at the Somerset County Department of Health building to get a free hepatitis A vaccine, the outlet reported.
The virus, which is spread from person to person or in food-borne outbreaks, causes a highly contagious liver disease that can be fatal. Many people think it only affects the homeless or drug users, but anyone who isn’t vaccinated can be infected when exposed to contaminated food or drink.
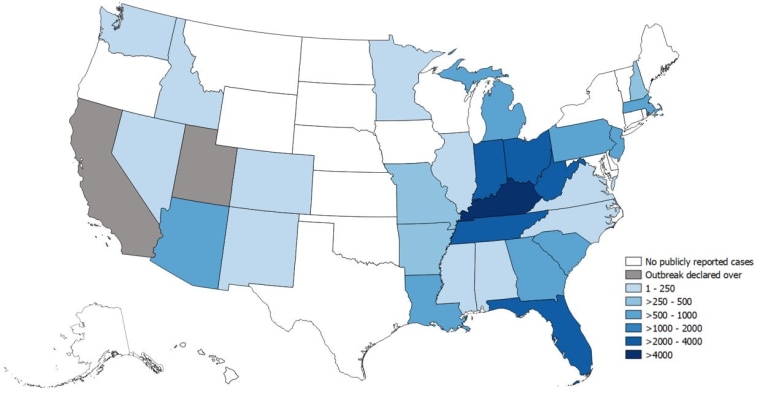
In August, Florida and the city of Philadelphia both declared public health emergencies after seeing a spike in cases. Other states are concerned, too, including Minnesota, Tennessee and Ohio.
Florida took the step to “alert the public to this serious illness and prevent further spread," said the state’s Surgeon General Dr. Scott Rivkees in a statement. So far this year, 2,970 hepatitis A cases have been reported in Florida, or more than five times the number of cases in 2018.
Who is at risk for hepatitis A?
Across the U.S., the Centers for Disease Control and Prevention has been monitoring “widespread outbreaks” of hepatitis A since 2016, with 27,634 cases and 275 deaths in 30 states as of Nov. 1.
“When thousands of people are infected with the virus that could eventually kill you, that’s an epidemic that’s worrisome,” Dr. Paul Offit, an infectious disease expert and director of the Vaccine Education Center at Children's Hospital of Philadelphia, told TODAY.
“The average person is at risk by walking into a restaurant where a food handler who has hepatitis A doesn’t adequately wash their hands and then makes and serves food.”
The virus is transmitted primarily by the fecal-oral route: It’s shed in the stool of infected people, who can carry it on their hands after going to the bathroom. If they prepare a salad, touch food on a plate or even hand out menus, they can then infect restaurant patrons. The virus is “very hardy” and lives well on surfaces, Offit said.
More than a dozen restaurant workers in Florida have been infected with hepatitis A so far this year, the South Florida Sun Sentinel reported, which may be particularly worrisome in a state that attracts tourists from all over the country and the world. The latest case involves two people who worked at a Denny's restaurant in Kissimmee.
“Each restaurant worker is potentially exposing hundreds or thousands of people to hepatitis,” William D. Marler, a food safety lawyer, told the newspaper.
“They don’t know they’ve been exposed and now they go back home and expose people there.”
Infected food workers continue to cause concern in other parts of the country. Eateries in New York, Georgia, Virginia, Missouri, Arkansas and Idaho are just some of the places where contagious employees may have recently put customers at risk.
The National Restaurant Association has taken notice, recommending that restaurants encourage employees to get vaccinated, educate them about the virus and monitor them for symptoms.
Frozen berries and produce imported from countries where there isn’t a great separation between sewage and drinkable water are another worry, Offit said. The fruits and vegetables can be sprayed with water that contains hepatitis A and be contaminated that way. The latest incident happened in October when frozen raspberries were recalled over contamination fears.
An outbreak of hepatitis A linked to smoothies made with frozen strawberries from Egypt sickened 70 people in 2016.
Still, the people most at risk are the homeless and drug users, with the homelessness issue most likely to blame for the spike in cases in recent years, Offit said. But that may fuel more infections since people in this population often gravitate toward lower-skill work, including the restaurant industry — particularly fast food, Marler told the South Florida Sun Sentinel.
Hep A symptoms and treatment:
Symptoms usually start within 28 days of exposure, but may take up to 50 days to show up. They include:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Diarrhea
- Clay-colored stools
- Joint pain
- Jaundice
There is no specific treatment other than rest, adequate nutrition, and fluids, according to the CDC. Unvaccinated people who know they may have recently been exposed to the virus should get the hepatitis A vaccine or a shot of immune globulin to prevent severe illness. Most people who are infected get better over time, but may need to be hospitalized.
How to protect yourself:
Get the vaccine: The only way to be truly protected is to be vaccinated. Hepatitis A rates in the U.S. have fallen by more than 95% since hepatitis A vaccine first became available in 1995, the CDC noted. The vaccine is given in two shots, six to 18 months apart.
The CDC recommends that all children be vaccinated, with the first dose given at 1-2 years of age. In June, the agency’s Advisory Committee on Immunization Practices also advised that kids 18 years old and younger who haven’t already received the vaccine should get it at any age.
Adults wishing to obtain immunity can get the vaccine at any time. “There’s no down side to getting it, it’s a safe vaccine,” Offit said. The CDC does not recommend booster doses, but getting extra doses is not harmful, it noted. People who have already had hepatitis A in the past won’t be infected again.
Practice good hand hygiene: It’s key to wash your hands with soap and running water for at least 20 seconds before preparing, serving or eating food. The virus is common in places where there are poor sanitary conditions or poor personal hygiene. Alcohol-based hand sanitizers do not kill the Hepatitis A virus.