This story discusses suicide. If you or someone you know is at risk of suicide please call the U.S. National Suicide Prevention Lifeline at 800-273-8255, text TALK to 741741 or go to SpeakingOfSuicide.com/resources for additional resources.
When it comes to recognizing depression in teens, it’s a tale of two realities for families, a poll released Monday has found.
Almost all parents, 90%, said they were either very confident or somewhat confident they’d know if their child was depressed.
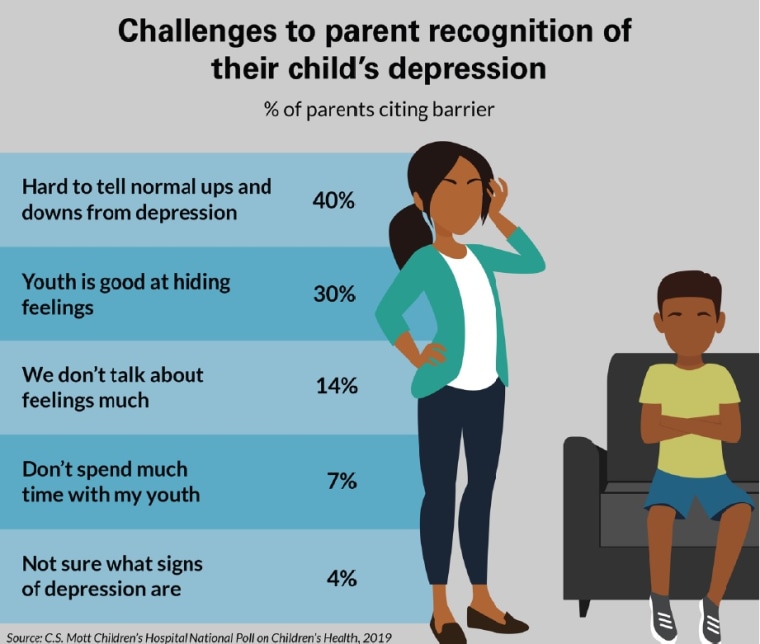
But two-thirds also admitted there were real challenges in recognizing the mental illness, including having a hard time telling whether a teen was experiencing normal mood swings or depression. They were also frustrated that adolescents were good at hiding their feelings.
The C.S. Mott Children’s Hospital National Poll on Children’s Health was based on responses from a nationally representative sample of 819 parents who had at least one child in middle school, junior high or high school.
The findings may appear conflicting, but they reflect the unease parents feel right now, said Sarah Clark, the survey co-director and a pediatrics research scientist at the Susan B. Meister Child Health Evaluation and Research Center in Ann Arbor, Michigan.
Parents educate themselves about the symptoms of depression, but then see grieving families in their communities who did the same thing and still missed the signs that their child was suicidal.
“It seems weird, like how can parents be confident and recognize these barriers at the same time? Parents are saying, ‘I think I would notice, but here’s a family — they seem like us — and those parents said they didn’t know until it was too late in some cases,’” Clark told TODAY.
“So parents realize that maybe recognizing this situation isn’t as easy as just knowing what the warning signs are.”
Suicide rates among young people are rising, reaching the highest levels since 2000, a study published in the Journal of the American Medical Association in June found. Suicide is one of the leading causes of death among adolescents 15–19 years old.
"I think what you’re seeing is a reflection of an incredibly stressed-out group of kids," Jonathan Singer, president of the American Association of Suicidology, a nonprofit that advocates for suicide prevention, told NBC News.
One in four parents said their son or daughter knows a teenager with depression, and 10% revealed their child knows a peer or classmate who died by suicide, the new poll found.
Almost three-quarters of parents thought their child’s school should screen all students for depression, and almost half said the screening should begin in 6th grade.
Signs of depression can vary from child to child, but these are classic ones parents should know about:
- Lack of interest in things and activities the teens once enjoyed.
- Any changes in behavior, including, appetite, energy level, sleep patterns and academic performance.
- Acting really sad or irritable.
- Complaining about being tired or having stomach aches (common in young children).
- Using words such as “down” or “stressed” rather than “depressed” — teens may use confusing language to describe their feelings, so take note of statements like "I always find somehow to go back to stressful mode” or “I get really mad at people very easily.”
- Any talk about suicide, even in passing.
- Giving away belongings.
The best way to get kids to talk is to just be present, said Jennifer Hartstein, a clinical psychologist who specializes in working with suicidal adolescents.
“Don’t be afraid to say, ‘You seem a little bit down today. What’s going on?’” she said. Don’t be afraid to ask your kids if they’re feeling suicidal, she added.
Kids are more likely to open up if you walk with them, so suggest a stroll rather than a formal face-to-face conversation, Hartstein suggested. If they’re not willing to talk now, tell them you’ll check back with them later and do it.
Most parents, 85%, thought their child would ask them for help if feeling depressed. Still, families should identify a “go to” adult — perhaps a teacher, coach or relative — who the teen can talk to outside the immediate family, the new report advised.
“There are times where the parent isn’t the first person a kid will talk to,” Clark said.
“You want to make sure that your kid knows, ‘Yes, you have my permission to do this — talking with somebody when you are feeling overwhelmed is a good thing to do. Don’t hide it, don’t feel like you have to handle the whole world by yourself. I’m here to help, but if you ever feel like you can’t talk to me, let’s figure out who you should talk to.”

