Women have different symptoms of heart disease than men do, and those differences can make for deadly mistakes, according to the American Heart Association.
The problem is compounded by the fact that in some cases, women don't know they're having heart issues. They are wary of visiting their doctors because they're afraid of being body-shamed, said Dr. Jennifer H. Haythe, the co-director of the Women's Center for Cardiovascular Health at the Columbia University Medical Center and a cardiologist at New York-Presbyterian hospital.
Women, she said, are "afraid to get on the scale. That's common, but it's not okay, and above all else, it's dangerous. If you feel that you are being body-shamed by your physician, you need to get a new one. Another reason women avoid checking their heart health is that there is this stigma with heart disease. When we think heart disease, we think: lazy, fat, smokers. We have to overcome that stigma."
The key thing to keep in mind, said Haythe: "Measuring your heart health has nothing to do with how new and shiny the car is. It's to check how well the engine is functioning."
Heart disease, said Haythe, is viewed as a "men's disease." So much so that often, women write off symptoms like feeling winded, palpitations, and dizziness as a "panic attack."
Although experts have known for years that women have different symptoms of heart disease than men do, the message still isn’t getting through to women — or the health professionals who treat them, according to the Heart Association.
That’s in large part because different factors can cause heart disease in women, and the focus has been largely on what happens in men, the group said.
“Despite stunning improvements in cardiovascular deaths over the last decade, women still fare worse than men and heart disease in women remains underdiagnosed, and undertreated, especially among African-American women,” said Dr. Laxmi Mehta, director of the Women’s Cardiovascular Health Program at The Ohio State University.
Mehta led a team writing the American Heart Association’s first statement focused strictly on women and heart disease.
Women don't get lifesaving medications
Most heart attacks are caused by blocked arteries in both men and women. But they can differ in how they form.
“Compared to men, women can have less severe blockages,” the Heart Association said. But they still damage the big arteries that bring blood to the heart.
“The result is the same— when blood flow to the heart is decreased for any reason, a heart attack can occur,” the group said. That adds up to 53,000 women dying from heart attacks every year.
“If doctors don’t correctly diagnose the underlying cause of a woman’ heart attack, they may not be prescribing the right type of treatments after the heart attack.”
That means women often don’t get lifesaving medications. The result: More women than men die within a year of their first heart attack — 26 percent of women versus 19 percent of men.
And 40 percent of people who die suddenly from a heart attack or other severe heart event are women.
Women also tend to have smaller blood vessels to start with, they’re older when they have heart attacks than men are and more likely to have other conditions such as diabetes and high blood pressure.
Women with high blood pressure are more likely than men with high blood pressure to have heart attacks, and if a younger woman has diabetes, her risk of a heart attack is four to five times higher than it would be for a young man with diabetes.
Women wait too long for help
And their symptoms are different.
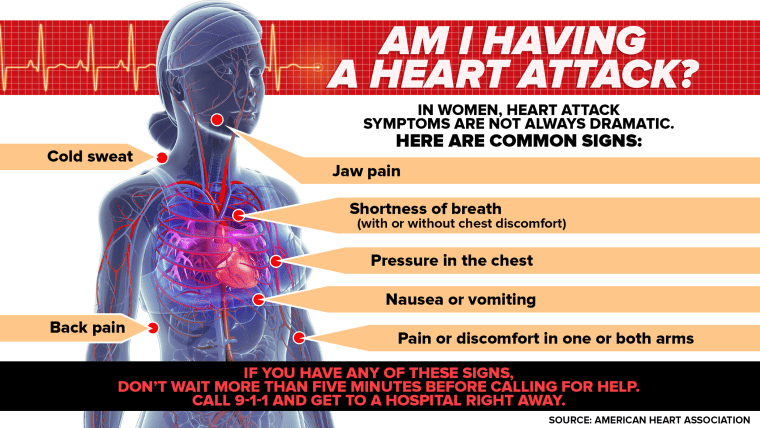
“While the most common heart attack symptom is chest pain or discomfort for both sexes, women are more likely to have atypical symptoms such as shortness of breath, nausea or vomiting, and back or jaw pain,” the Heart Association said.
“Shoulder pain and arm pain are twice as predictive of an acute coronoary syndrome diagnosis in men compared to women.”
“Most heart disease research is done in men, so how we categorize it is based on men. We need more science in women.”
That means women might not realize they’re in trouble and wait too long to see help. A man usually shows up in the emergency room within 15 hours of first symptoms. On average, it takes U.S. women more than two days.
So it's imperative that women speak up. Until they're heard.
"You know if you're feeling off and something is wrong. Don't write it off, and don't feel pressured to write it off," said Haythe.
Her advice:
- Listen to your body.
- Go to your doctor.
- If you feel that you are having a panic attack, and you do go to the doctor or hospital, tell them: "I want my heart to be checked to make sure it's not a heart attack."
Once you voice that, they will have to check out your heart health. You have nothing to lose by being extra cautious," said Waythe.
Researchers have reported that heart attacks can be deadliest for young women. If a young woman has a heart attack, she is more likely to be sicker than a young man and more likely to die in the hospital.
“Over the last 10 years or so, we’ve learned that women’s hearts are different than men’s in some significant ways, and while that’s helped reduce mortality, there’s much more to know,” said Mehta.
“Most heart disease research is done in men, so how we categorize it is based on men. We need more science in women.”
Common heart attack symptoms in women:
- Pain in the upper back, neck or jaw
- Indigestion
- Nausea
- Palpitations
- A sense of dread
This story was originally published on Jan. 26, 2016.