About a year ago, Ann Heslin experienced "incredible burning pain" on her vulva and discovered two ulcers on her labia. She told her dermatologist about it — her father had died of skin cancer and she feared that’s what she had.
“It took a lot of courage for me to ask her to look at such a private area. But I was in so much pain that I needed to get some resolution,” Heslin, 44, director of special philanthropic events at Ochsner Health in southern Louisiana, told TODAY. “In my heart, I knew I had cancer.”
Her doctor eventually diagnosed her with vulvar cancer, a rare gynecological cancer. She’s sharing her story to encourage people to speak up when they notice something wrong — even if it is in a sensitive area.
“It’s kind of embarrassing, honestly, to ask your doctor to look at these two ulcers that you have and you think, ‘Oh gosh, how did I get that?’” she said. “I really want my story … to be something that other people can benefit from.”
Unusual symptoms
After finding the ulcers in January 2021, Heslin wondered if she had been burned during a recent waxing appointment. But she waited for her upcoming skin check with her dermatologist to mention it.
“(My doctor) said, ‘Well I think you have a sexually transmitted disease,’ and I said, ‘I really don’t think I do. I think that this is skin cancer,’” she recalled. “I said ‘Well my dad passed away from squamous cell carcinoma … in his left sinus cavity in 2010 and this looks similar to what my dad had on his face.'”
Her doctor tested her for STIs and Heslin was negative. She did test positive for bacteria so she started taking an “aggressive course of antibiotics and steroid cream.”
“Nothing was working. It was just getting worse and worse,” she said. “Every day I’d think, ‘Today is the day that these two ulcers go away.’ I was in so much pain.”

But various antibiotics and steroid creams did nothing. By March, Heslin struggled with even taking a few steps.
“I could not walk,” she said. “I was frankly very desperate for the solution.”
She returned to her dermatologist who urged her to do a biopsy for vulvar cancer and the results indicated that she had squamous cell carcinoma. While Heslin was relieved to have a diagnosis, it brought back tough memories.
“My dad had a very short cancer journey … five months from diagnosis until the day he died,” she said. “Everybody in my family was concerned. I cried. My sister cried. My mom cried.”
She met with Dr. Katrina Wade, a gynecologic medical oncologist at Ochsner. Heslin had surgery to remove the cancer and a nearby lymph node.

“I was very shocked, a little disappointed that it went from stage 1A on the day of surgery to stage 3,” she explained. “I had a lot of reconstructive surgery. Dr. Wade did an incredible job. But because of my tumor, its location, its depth, its (stage) and the margins, it was very extensive surgery.”Eight weeks after surgery, she had six weeks of chemotherapy and then “27, 20-minute rounds of radiation.” Grappling with skin changes and pelvic floor pain from the radiation has been tough, but Heslin has gone to pelvic floor physical therapy and received other treatments to help.
“You have so many skin changes that occur when you have radiation. So there are lots of different things that you have to do to maintain the health of your skin,” she said. “One thing that I think helped me out tremendously, and still is helping me out tremendously, is acupuncture.”
Vulvar cancer
According to the National Cancer Institute, about 6,120 people were diagnosed with vulvar cancer in 2021. About 0.3% of people with vulvas will be diagnosed with this cancer in their lives. While vulvar cancer is rare, knowing the signs and when to talk to a doctor leads to earlier diagnosis and often a better outcome.
Symptoms can include:
- Chronic itching or burning of the vulva or labia.
- Skin changes, a whitish, pink or black tint that looks different than normal skin.
- An ulcer or sore that doesn’t heal.
“Some people might (think of) a yeast infection where they have a lot of itching and burning,” Wade told TODAY. But she added that vulvar cancer symptoms would be “persistent (and) don’t resolve in what you think of as the normal way.”

Vulvar cancers are skin cancers that occur on genital skin.
“It’s something that’s not necessarily associated with sun exposure,” Wade said. “The types of cancer that occur on the vulva are very similar to the type of cancers that occur on other parts of the skin so squamous cell carcinomas, basal cell carcinomas and even melanomas account for 10% of vulvar cancers.”
The risk factors for developing vulvar cancer include:
- Having HPV.
- Being a smoker.
- Having a skin condition that cause chronic inflammation, such lichen sclerosus.
Lichen sclerosus is a rare condition that causes “chronic nighttime itching of the vulva," most commonly affecting people before puberty or after menopause.
“Just because someone has lichen sclerosus, they’re actually not likely to develop vulvar cancer,” Wade said. “But it’s certainly a risk factor. Lichen sclerosus is easily treatable and controlled with the same things we treat other skin conditions, which are topical steroids.”
Heslin had learned she has the condition and uses medications to manage it.
Like other cancers, catching vulvar cancer early leads to better outcomes. Wade urges people to speak to their doctor if they notice any changes.
“I also encourage patients to know their own anatomy. Just like we teach women about self breast examination you should know what your skin looks like in all areas of the body, even the private ones,” Wade said. “You can notice any early changes that might be new or different.”
Life after treatment
After three months of treatment, Heslin underwent a PET scan and learned she was cancer-free in October 2021. She had another appointment last week that showed she is still doing well. While she had a flare up of her lichen sclerosus, she’s focused on putting it into remission. Prior to having cancer, she ran five days a week. She’s not back to that just yet, but she’s trying to do what feels right for her.
“My stamina is continuing to rebuild itself,” she said. “I’m the type of person who wants to continue to challenge myself and get better every single day so I continue to challenge myself with my runs —eventually I’ll get back to where I was before I had cancer.”
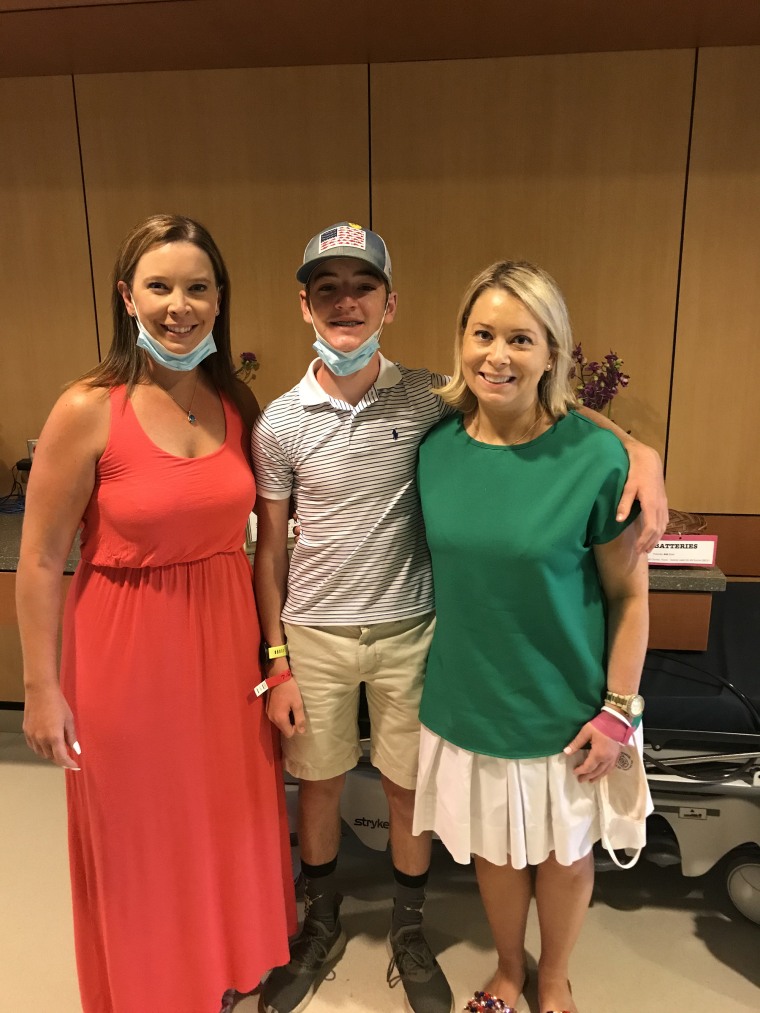
Support from family and friends helped her throughout her treatment and she feels grateful for the love she received. She hopes her story will help de-stigmatize vulvar cancer.
“There’s nothing to be ashamed of — your skin is your largest organ in your body. So I happened to have skin cancer on my vulva,” she said. “All cancers are important and I really hope that by sharing my story it will encourage other people (to seek help).”
Related:
