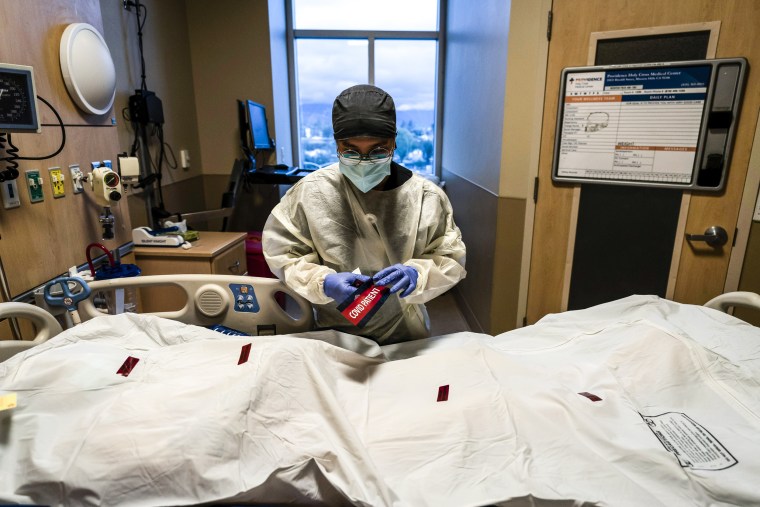
One million people have now died in the U.S. because of COVID-19, according to NBC News' latest tally.
It would have been impossible to imagine that death toll just over two years ago, when the novel coronavirus began spreading around the world.
Even after the grim first wave swept through New York City in the spring of 2020, the national lockdown that followed and the surges that keep claiming lives, one million U.S. dead is still hard to grasp.
Yet here we are.
The death toll didn’t have to be this bad, and the pandemic response could have been much better handled, said Dr. Amesh Adalja, a senior scholar at the Johns Hopkins University Center for Health Security in Baltimore and spokesman for the Infectious Diseases Society of America.
“All of this is a lesson for how a country that was considered the most prepared for an infectious disease emergency or a pandemic, even if they’ve got the greatest toolbox and the greatest minds … could still end up with a horrendous death toll,” Adalja told TODAY.
“The number would be much higher if it were not for vaccines. … We would be in horrible shape.”
Americans aren’t numb to the huge number, but “it’s not necessarily something that they can wrap their minds around” because the deaths happened over two years, and people have been through so much, he added.
Mistakes from the start
Adalja believed some of the biggest mistakes happened at the start of the pandemic in early 2020, when the government chose “evasion” rather than a proactive approach, giving the virus a head start to spread, he said.
Timely and widespread testing was crucial to isolate infected people, but there were constant problems including faulty test kits, delayed test results, bottlenecks in labs and long lines at testing sites before at-home COVID tests became available. Frustratingly, testing issues have lingered, with problems continuing during the recent omicron variant surge, Adalja noted.
There’s also been minimal investment in public health infrastructure and hospital capacity, leading to recurring problems “as if this was coming out of the blue,” he added.
“The biggest mistake has been to allow politicians to be in charge of the response,” Adalja said. “We need pandemic preparedness and the CDC to be more independent.”
Impact of vaccines
The COVID-19 vaccines saved almost a quarter-million lives and prevented almost 1.2 million hospitalizations in the first six months of 2021, according to a model published in January in JAMA Network Open.
But there could have been even greater impact if more people were vaccinated, experts told NBC News.
Adalja was surprised by the vaccine hesitancy, noting it has led to many preventable deaths. Not enough people at high risk for severe COVID-19 have gotten vaccinated, he said. That’s one of the issues driving deaths now, in addition to a lack of access to treatments like Paxlovid and monoclonal antibodies, he added.
About 82% of people in the U.S. have received at least one dose of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention. More than half of people in the U.S. had COVID-19 by the end of February, the CDC found after testing for specific antibodies that develop only after an infection.
The concern now is how well the vaccines will continue to prevent people from dying. A recent investigation by the Washington Post found a rise in deaths among the vaccinated, especially older adults and those who didn’t get a booster shot.
“This virus preys on the elderly — that’s what we’ve seen from the very first days of this pandemic,” Adalja said. “That’s why it’s really important for elderly people to be up to date on their vaccines and if they get sick, to contact their doctor as quickly as possible.”
Looking ahead
More than two years after the horrendous COVID-19 death toll began in 2020, there are reasons for optimism. The virus is much more manageable now, and even when people become infected, there is less need for hospitalization, Adalja said.
“It’s unlikely to see hospitals get overwhelmed again because the population has so much immunity from infection and from vaccination, as well as access to monoclonal antibodies, antivirals and rapid tests,” he noted.
“(But) there will be more variants coming till the end of time. That’s just what coronaviruses do. … We’re not going to be back in 2019, ever.”
The goal now is to boost people who are at high risk for severe disease and develop second-generation vaccines that don’t require boosters so frequently, Adalja said.
