A newly approved drug intended to slow the progression of Alzheimer’s disease offers patients hope, but it will come with a steep price tag: $26,500 a year.
The drug, called Leqembi from the drugmakers Eisai and Biogen, was approved by the Food and Drug Administration on Friday for use in people with mild cognitive impairment or early Alzheimer’s disease.
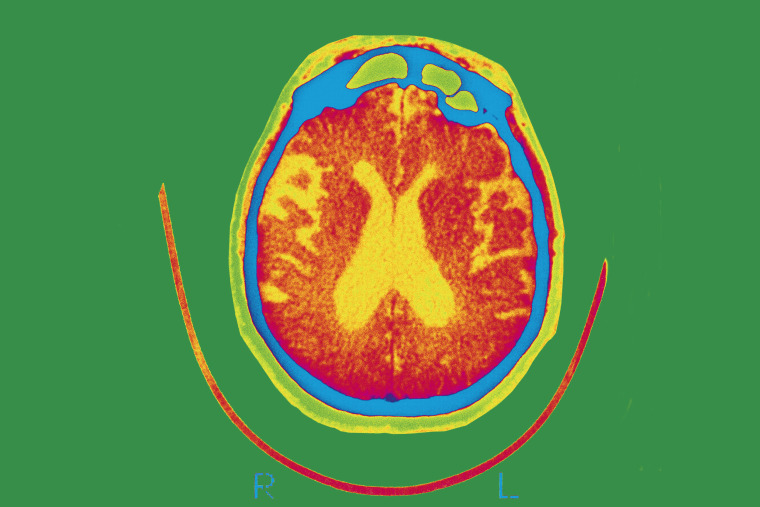
It’s only the second drug approved in the United States — behind Biogen’s Aduhelm — aimed at attacking what is thought to be one of the underlying causes of the disease — build-ups in the brain called amyloid plaques.
Leqembi’s annual price tag of $26,500 is below the price set for Aduhelm — which was approved by the FDA in 2021 despite strong objections from its panel of outside advisers. That drug initially cost $56,000 per year before Biogen slashed the price in half, to $28,000 annually.
Still, the price for Leqembi is much higher than recommended by the Institute for Clinical and Economic Review, a Boston-based research group that helps determine fair prices for drugs. Dr. David Rind, the institute’s chief medical officer, said an appropriate cost for the drug is $8,500 to $20,600 a year.
“We think this is overpriced right now,” he said.
Because of the high price tag, experts say, the number of people who will be able to get the drug when it becomes available — expected the week of Jan. 16 — will be extremely limited. More than 6 million people in the U.S. have Alzheimer’s disease, according to the Alzheimer’s Association.
As a rule, the Centers for Medicare & Medicaid Services restricts coverage for new Alzheimer’s treatments that target amyloid, including Leqembi, to only those patients participating in clinical trials.
John Domeck, 60, of Aurora, Ohio is currently enrolled in a phase 3 clinical trial testing Leqembi. Because of that, he gets the medication free every two weeks.
But his wife, Ann Domeck, says she doesn’t know if that will continue when the trial ends in the next two years, even though John qualifies for Medicare.
“I don’t know if we could afford it,” she said, “but we’re going to cross that bridge when we come to it.”
Holly Fernandez Lynch, an assistant professor of medical ethics at the University of Pennsylvania, said the CMS standards for covering new Alzheimer’s treatments are higher than those the FDA uses to get new treatments on the market quickly.
Leqembi was approved under the FDA’s accelerated pathway, which allows early approval for new drugs that “fill an unmet medical need” and are found to be safe and effective. In its review for accelerated approval of Leqembi, the FDA looked at data from a phase 2 clinical trial of more than 800 patients. Eisai and Biogen will still need to submit data from an additional phase 3 clinical trial that confirms the benefits of the drug to gain full approval.
“The standard for CMS coverage is not that the drug is safe and effective,” Lynch said. “It is that ‘is it reasonable and necessary for the Medicare population.’”
Lynch said the CMS can’t determine that until it has seen the full data from both clinical trials.
Arthur Caplan, the head of the Division of Medical Ethics at NYU Langone Medical Center in New York City, said the CMS has to be especially cautious about what medications it covers because drugs, like Leqembi, could cost it billions. About 6.5 million people over the age of 65 have Alzheimer’s and would qualify for Medicare.
The CMS may be willing to swallow that cost if the drug is shown to provide a lot of benefits for patients, he said.
But right now, the clinical trial for Leqembi shows that the drug provides “modest efficacy at a big, big price,” Caplan said.
It’s possible, Lynch said, that the CMS will consider covering Leqembi once the drug receives full approval. Eisai announced late Friday that it had submitted an application for full approval. Ivan Cheung, the U.S. chairman and CEO of Eisai, told NBC News that the FDA could reach a decision in six months.
But, as of right now, it appears the CMS is unwilling to budge on its policy stance, Lynch said.
“The CMS has said, ‘Look, something might be safe and effective from the FDA’s perspective, but we have too many qualms about the qualify of evidence,’” she said.
In the meantime, many patients who want the drug will not be able to afford it, said Dr. Alberto Espay, a neurologist at the University of Cincinnati College of Medicine.
It’s “very unfortunate,” he said, noting that physicians will have to explain to patients the potential benefits — a modest slowing of the disease — alongside the risks, which may include a great financial burden.
This story first appeared on NBCNews.com.